Frozen Shoulder
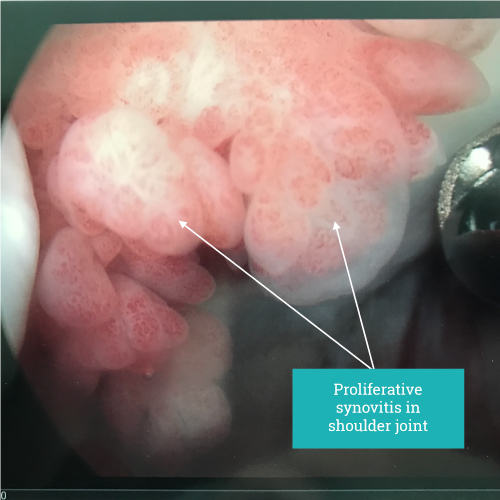
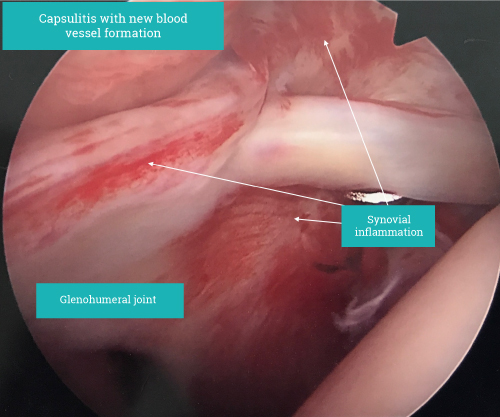
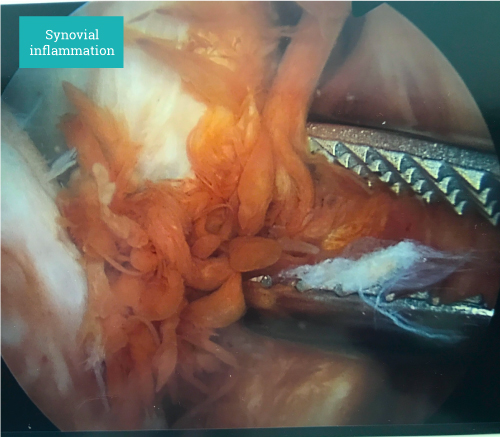
The underlying problem is inflammation of the glenohumeral joint ie capsulitis.
Most commonly a cause is not found. Anything that produces inflammation in or around the shoulder make provoke glenohumeral inflammation. Commonly seen associations are acromio-clavicular joint inflammation, trauma ranging from relatively minor tendon or labral injury to fractures and dislocations. Surgery also commonly will precipitate a frozen shoulder.
Other causes of inflammation in joints such as rheumatoid arthritis or other inflammatory arthropathies can bring about the symptoms of a frozen shoulder.
Typically a frozen shoulder occurs between the age of 30-60 being seen more commonly in men than women.
The most important key to a frozen shoulder is that it is by its nature a self-limiting condition. That is to say it follows a typical course and burns out with near complete resolution.
A typical frozen shoulder may come about insidiously some weeks after a minor injury first being noticed with pain at night or when overreaching. This can be very mild or develop to a point where pain at night is causing significant lack of sleep and all movements are restricted.
Maximum loss of movement results in being able to elevate the hand to shoulder height only, being unable to rotate the shoulder for example reach behind the back and struggle to bring the arm away from the side.
All extremes of movement in particular sudden movements may provoke severe pain down the entire arm lasting a few minutes. (reaching to catch a falling object, reaching into a low cupboard, car boot pulling arm up, stretching after waking). Over time the night pain stops, stretching becomes painfree but limited and then movement will return. This all takes 8-12 months on average.
Treatment is aimed at pain management. We typically recommend image guided (either ultrasound or x-ray) intra-articular steroid injection. Image guidance increases greatly the probability that the glenohumeral joint is targeted.
Simple subacromial injection whilst much easier to deliver without guidance is not as effective for a frozen shoulder. If this is done at three months after onset the pain may recur and a second injection will help. If the injection is first done about 6 months after frozen shoulder symptoms started it will typically be enough to resolve pain. Steroid injections have only a small effect on the stiffness and this will run its course and return to normal.
Many other treatments have been proposed. With increasing complexity comes an increasing risk of complications. Treatment such as hydrodistention, manipulation or arthroscopic release under anaesthesia have a 5 % risk of significant complications. Although short term the shoulder may be improved at 6 -12 months outcome is the same. In our practice these procedures are reserved for the few individuals who fail to resolve symptoms after conservative management (1-2%).
Physiotherapy on the acutely painful shoulder is frustrating for both the patient and therapist as the stiffness fails to respond and increasing pain can be a problem. In the acutely painful stage physiotherapy on the periscapular muscle and cervical spine can be a help as these areas will often become painful secondary to the abnormal movement of the frozen shoulder.
Once the pain has started to resolve physiotherapy working on regaining movement in the shoulder itself may be of benefit. If however this is to painful or if pain increases after treatment then wait eight weeks and then try again.
“Typically a frozen shoulder occurs between the age of 30-60 being seen more commonly in men than women.”
Make an appointment
If you wish to make an appointment to discuss your needs further, please get in touch.
Hermitage Medical Clinic
Old Lucan Road
Dublin 20
Call for appointments: 01 6459562
Telephone: +353 1 645 9000
Fax: +353 1 645 9235
Email: info@johnlunn.ie