Shoulder Injections
Injections are used to deliver drugs such as steroids to the site of the problem. This allows higher doses of the drug to reach the target whilst avoiding side-effects that occur when the drug is taken systemally (ie tablet form). Drugs used all act by a predominantly anti-inflammatory mechanism. The most commonly used are corticosteroids which are powerful anti-inflammatories.
There are three separate spaces around the shoulder that in normal circumstances do not communicate with each other.
1) The acromio-clavicular joint
2) The sub-acromial space
3) The Glenohumeral joint
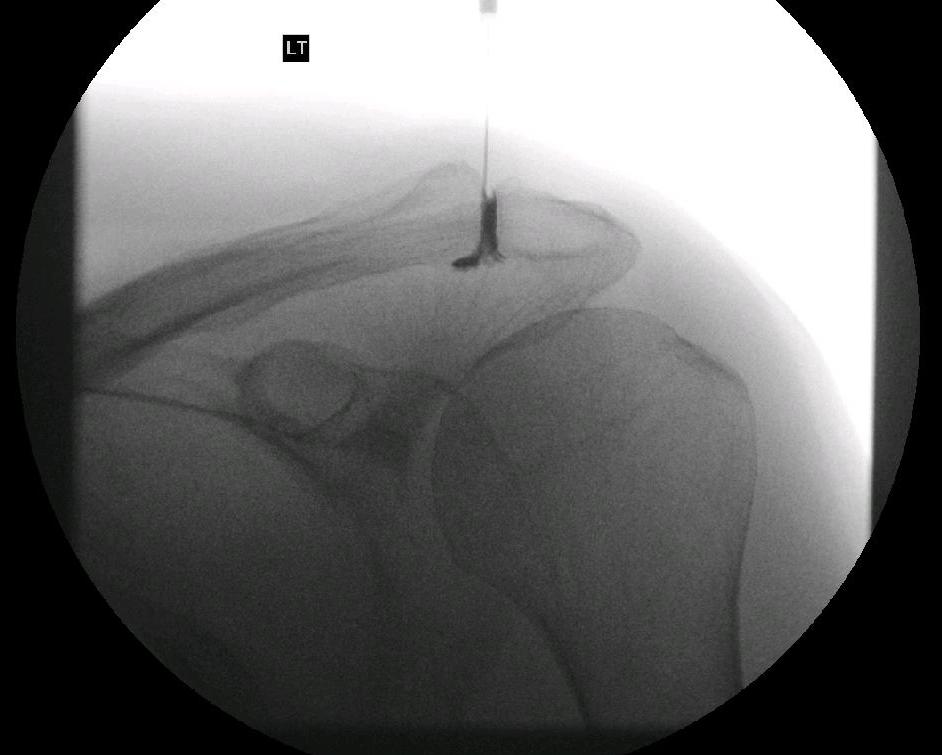
Depending on the problem the injection is targeted to the affected area. The subacromial space is easily injected. This is frequently done in an outpatient setting and rarely requires image guidance. The AC joint and the Glenohumeral joints are less reliably injected unless image guidance is used (typically x-ray or ultrasound)
What is injected?
We use Marcaine as a local anaesthetic this gives short term pain relief for approximately 12 hours.
The primary drug is a long acting steroid. We use Depomedrone. This reduces inflammation and vascularity which is a source of pain in most problems.
When injecting into the Glenohumeral joint we use Omnipaque (Iohexol). This is an iodine based solution which shows up on x-ray allowing us to confirm we are in the correct place for injection.
What are the risks and complications?
Allergic reactions are rare but can be serious. They usually occur within minutes of the injection. Symptoms range from a skin rash, vomiting to swelling of the mouth and lips and in extreme cases shortness of breath and difficulty breathing. This requires immediate medical attention. A person who is allergic to Iodine should avoid omnipaque as this contains iodine.
Skin flushing is common and lasts a few hours.
Fat necrosis or loss of pigment. Rare. If any steroid escapes from the shoulder joint into the soft tissues around the shoulder you can get a dimple and or whitening of the skin. This can be permanent.
A Flare of pain occurs in around 10-30% of injections this can last 2-3 days before it resolves. If you had a flare of pain from a previous injection you are likely to experience the same reaction with further injections.
Deep infection. (very rare after injection). This occurs 1 in every 1000-10,000 people having an injection in the shoulder. If you get a deep infection in the shoulder you are likely to be worse than when you started with a possibility that the shoulder will be permanently damaged. Infection may be hard to diagnose initially as the joint is already painful and a flare of pain is often seen after an uneventful injection. Pain increasing after 3-4 days with, swelling, redness, pus at the site of the intervention or systemic symptoms such temperature elevation and generally feeling unwell should raise the possibility of an infection . A simple blood test is helpful (C-Reactive protein and Full blood count).
What to expect after an injection around the shoulder.
The local anesthetic should reduce pain for several hours immediately after an injection. This is very useful for confirming a diagnosis as reduction or disappearance of the pain even if only for hours confirms that the pain is from the area injected (Not referred from the neck or elsewhere in the shoulder).
Once the local anaesthetic wears off the pain may return.
10-30% of injections will provoke a flare of pain lasting 2-3 days. If this occurs rest the arm, use ice wrapped in a thin towel over the site for several minutes every hour. Take pain relief typically over the counter paracetamol and an anti-inflammatory are sufficient. The Steroid takes 1-2 weeks to start to reduce pain.
The main goal is pain reduction. Steroids will not help a torn tendon to heal or reverse arthritis in a joint. Stiffness associated with a frozen shoulder resolves spontaneously over time with or without an injection.
“Drugs used all act by a predominantly anti-inflammatory mechanism.”
Make an appointment
If you wish to make an appointment to discuss your needs further, please get in touch.
Hermitage Medical Clinic
Old Lucan Road
Dublin 20
Call for appointments: 01 6459562
Telephone: +353 1 645 9000
Fax: +353 1 645 9235
Email: info@johnlunn.ie